FSG Managing Director Nikhil Bumb asks a question during a lunchtime panel at the FORTUNE Brainstorm Health 2023 conference. Photograph by Stuart Isett/Fortune.
Uncertainty is the new normal, and health care leaders know this reality particularly well after the past few years. FSG was invited to participate in FORTUNE’s Brainstorm Health conference, an annual convening of experts from a variety of industries and sectors to talk about the changing landscape of health care and the vital role of business to shape what comes next.
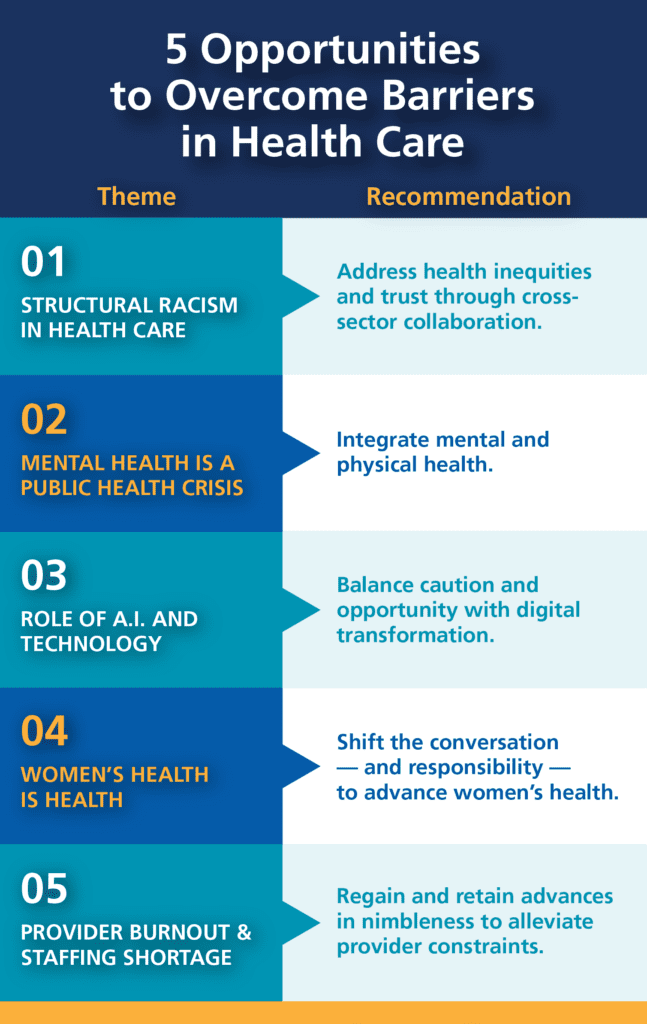
The conference was rich with insightful conversations about trends in health care—what’s pushing the frontier and what’s holding us back. Here are five takeaways that stuck with me, followed by 5 opportunities for companies to shift approaches and positively impact these challenges in the face of ongoing uncertainty:
1. Structural racism in health care
One of the most powerful—and memorable—sessions was on “Black Maternal Health: Reversing the Mortality Crisis.” The U.S. has the highest infant mortality of any industrialized nation. Black women are 3x more likely to die from a pregnancy related complication than White women. These poor outcomes are directly linked to differential access to health care and, when there is access, racial bias in clinical care, in addition to being driven by social determinants of health and underlying structural inequities. Addressing these systemic issues will require going much beyond diversity in clinical trials and recognizing that, as Charles Johnson, founder of 4Kira4Moms said, “when we fix it for Black women, we fix it for everyone.”
2. Mental health is a public health crisis
U.S. Surgeon General Vice Admiral Dr. Vivek Murthy observed that “loneliness is a public health crisis.” This epidemic has been growing for decades before the COVID-19 pandemic, and only exacerbated by lockdowns, increased social media, and increases in remote work. The crisis is particularly acute among the increasingly young workforce; suicide is the number two cause of death among Americans ages 15 – 34.
3. Role of A.I. & technology
While the pandemic accelerated digital transformation in health, many large challenges still hold us back. The conversation examined significant advances in medical technology, including a live demonstration of a smart stethoscope from Eko that uses machine learning to diagnose lung and cardiac disease while age-old challenges persist, including a plethora of incompatible EHR/EMR (electronic health/medical record) systems.
4. Women’s health is health
Gender equity and women’s health came up in almost every session at the conference. Outside of cancer, only 10% of R&D spend in the pharmaceutical industry goes to women’s health. 80% of medical schools do not include menopause in their curriculum. Health tech investor Christina Farr of OMERS Ventures summed it up: “We are far too comfortable with women’s pain.”
5. Provider burnout and staffing shortage
Up to half of U.S. physicians and nurses were feeling burned out before the pandemic. Today, increased pressures and reduced resources are resulting in an alarming burnout crisis and shortfall of staff in clinical as well as academic settings to train the next generation of workers. And these challenges—burnout and staff shortages—are worse for providers of color.
The challenges discussed are by no means easy to solve, but it was invigorating to hear so many CEOs and leads of commercial business units across industries talk alongside government, academic, and nonprofit leaders about their willingness to and the vital role that companies can and should play in addressing them. Here’s what makes me excited and what I am bringing back to our work with health care and life science companies:
1. Addressing health inequities and trust through cross-sector collaboration and coordination
Lack of trust in the health system is an existential crisis acutely felt by health care professionals and sector leaders right now. But as Dr. Neel Shah, chief medical officer of Maven Clinic, notes: “It’s not the job of the people (patients) being served to be more trusting of us (providers and leaders). It’s the job for us to be held accountable to be trustworthy.” That requires working to earn the trust of community partners with established relational trust in underserved communities, making sure people are matched to service providers with an understanding of lived experiences and/or shared lived experience, and consistently showing up for people and community partners when needed and when they expect you to.
Cross-sector collaborations offer a way forward to address systemic challenges—like improving Black infant and maternal outcomes—through aligned, long-term visions and plans and coordinated interventions. Chelsea Clinton spoke about learning from the approach to address the HIV/AIDs crisis and the market shaping opportunity for public-private partnerships to address the greatest unmet health needs for marginalized populations. By working together across sectors (e.g., new regulatory frameworks alongside shifting payer reimbursement models from fee-for-service to value-based care) we can shift market dynamics from high-demand, low-access to low-demand, high-access and dramatically improve health outcomes.
2. Integrating mental and physical health
Traditionally mental and physical health have been separate departments in clinical care settings, often with little to no interaction. Indeed, many employee health benefit plans include little to no mental health coverage or have separate benefit providers and/or processes for mental and physical health. Yet the two are closely linked. Dr. Murthy spoke about how loneliness puts people at increased risk for heart diseases, dementia, and earlier mortality. As we see moves towards integrated care in other parts of the health system, there is both a need and a significant opportunity to integrate the way we talk about and create solutions for mental and physical health together.
3. Balancing caution and opportunity with digital transformation
Dr. Shah put it best: “An app isn’t going to fix health care.” Yet, there is an opportunity for business leaders to clearly define which health care burdens technology can alleviate (e.g., administrative load to create more time for patient care). While an app won’t solve issues like structural racism in health care—and A.I. and technology is rife with opportunities for bias—when used well, digital tools have the power to make health care more reliable and trustworthy. To do so effectively, particularly when thinking about A.I. and machine learning, it is important to identify upfront what training datasets you will use, how that data is collected, how long you have to train that data, and how you will continue to learn and monitor for bias.
4. Shifting the conversation—and responsibility—to advance women’s health
Reproductive health conversations and solutions are largely focused on women. We lack the same range of options for men as we have for women in both contraception and fertility treatments, which is a manifestation of an underlying mindset that women must shoulder the burden. We need to shift the conversation and, therefore, the responsibility so that women’s health is not seen solely as a “women’s issue” but one where men share the burden of advancing and improving outcomes.
5. Regaining and retaining advances in nimbleness to alleviate provider constraints
Robert Wachter, UCSF Department of Medicine chair, noted that while the pandemic unlocked rapid advances in nimbleness in the health system, we are seeing a regression in how the sector approaches care post-pandemic (e.g., walk backs in telemedicine licensing across state lines). As we look for opportunities to address provider shortages, burnout, and resource constraints amidst other uncertainties, we can learn from pandemic gains and advance on these innovations to build in unlock additional ways to alleviate pain points in the system.
* * *
Clearly, businesses across all industries—not just health care and life science companies—play a critical role in our broader health system. Companies that adopt a systems lens, center on equity, and work collaboratively with other sectors will be better positioned to address the largest health care challenges and present stability in times of uncertainty, while unlocking significant economic value for their stakeholders.