Several threads in the news lately connect to how health systems pivot from crisis mode to a sustained response. The countries affected by the Ebola epidemic are moving from an initial influx of technical advisers to emphasize longer-term strengthening of their health systems. Funders like The Global Fund to Fight AIDS, Tuberculosis and Malaria are adopting new mechanisms to address countries in transition from donor dependence to country ownership.
In 2000, Botswana was one such country in crisis. The HIV/AIDS epidemic was ravaging the country, with an adult prevalence rate over 28 percent. Projections from the World Health Organization (WHO) indicated that 85 percent of 15 year-olds in the country would eventually die of AIDS. At the United Nations, President Festus Mogae said, “We are threatened with extinction. People are dying in chillingly high numbers. It is a crisis of the first magnitude.”
Over the past 15 years, Botswana has made remarkable progress in its effort to curb the HIV/AIDS epidemic, reducing deaths due to HIV per 100,000 people from 1,082 in 2000 to 284 in 2012 (calculation based on deaths data from UNAIDS 2013 Global Report and population data from World Bank DataBank). One of the largest contributors to this reduction in HIV mortality in Botswana was the dramatic scale-up of the antiretroviral therapy (ART) program which today reaches an estimated 85 percent of those in need1. The African Comprehensive HIV/AIDS Partnerships (ACHAP), the first public-private partnership to tackle the HIV epidemic at a national scale in sub-Saharan Africa, contributed significantly to this success.
Public-private partnerships today remain a valuable contributor to tackling challenging health issues at scale in sub-Saharan Africa, but funders, governments, NGOs, and others still struggle to identify the right structure for engaging the private sector in a way that takes advantage of the private sector assets and allows the partnership to remain flexible and adaptable.
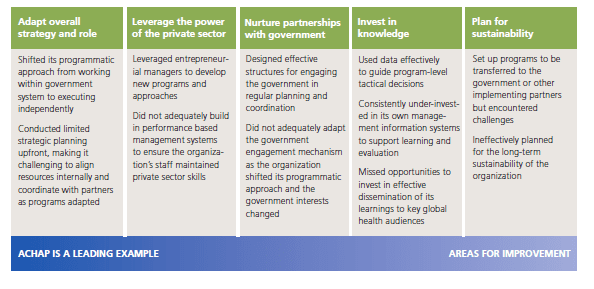
Over the past year, FSG has conducted an in-depth assessment of ACHAP’s performance over the last 15 years. Our assessment of ACHAP’s performance highlighted five critical characteristics for building successful public-private partnerships. ACHAP’s story is nuanced and we found that assessing ACHAP’s performance through the lens of these five characteristics allowed us to understand and highlight the challenges and complexities of managing a successful public-private partnership over time.
ACHAP’s performance against the five characteristics of high-performing public-private partnerships
ACHAP truly was a pioneer in scaling HIV treatment in Botswana, working with the government to achieve the first widespread HIV treatment coverage on the continent, and influenced the formation of key global partnerships such as the US President’s Emergency Plan for AIDS Relief (PEPFAR). We believe there is much that other public-private partnerships can learn from ACHAP’s experience and have outlined lessons in the full report that provide guidance for engaging with the private sector today.
For more on the lessons from ACHAP and the detailed story of ACHAP’s journey, please reference the executive summary and full report below.
Download the executive summary and report
- The executive summary highlights five characteristics of high-performing PPPs that emerged from the assessment, and key lessons for the field
- The full report for more detail on ACHAP’s inception, governance, decision-making, organizational structure, and examples of how it adapted specific programs in response to the changing context of the epidemic
The research and report were supported by The Merck Foundation and Merck & Co, Inc.
1The Government of Botswana is currently conducting an audit of its estimates of the number of people in need of antiretroviral therapy. Preliminary output from this analysis has indicated a coverage rate of approximately 85 percent. This process will also result in revisions to historical coverage rates based on changes in the methodology for estimating need.